Green nasal drainage–time for an antibiotic. Or is it?
Tis the season…for colds, strep, and flu. How can you tell when your kid has a common cold versus strep or the flu? Here is a quick rundown of the 3 common illnesses and how you can differentiate between them all. I have bolded things that are important and frequently mistaken or unknown.
- THE COMMON COLD
- Causes: Most commonly caused by rhinovirus, but there are >100 viruses that cause the common cold.
- Symptoms:
- Runny nose with clear watery drainage, often becomes thick, yellow or green in the first 3-7 days. This does NOT mean it’s bacterial or that “it’s a sinus infection and needs an antibiotic”.
- Cough
- Sore throat
- Stuffy nose
- Sneezing
- Low-grade fever (less than 101). Typically, fevers last less than 3-5 days.
- Feeling tired
- Decreased appetite
- Mild headache
- Symptoms usually begin 2-3 days after being exposed to the virus through droplets/contact with secretions (sneezing, coughing, kissing, shaking hands, shared toys or items). Symptoms get worse and peak around days 5-7, and usually last 7-10 days total. I’ll say it again: symptoms get worse until days 5-7 and usually last 7-10 days.
- Treatment:
- If your child only has a common cold and no complications, he will get better on his own in about 7-10 days. It will “run its course.”
- Antibiotics will not help and if you take them unnecessarily, they may not work against future infections.
- Encourage lots of fluids, rest, Tylenol (acetaminophen) or Advil/Motrin (ibuprofen) for fever or pain.
- Use a humidifier in their room or use the steamy shower to help loosen up nasal congestion/mucus and relieve cough.
- Use saline drops and bulb suction for infants/toddlers to clear their nose
- Give a teaspoon of honey for nighttime cough if your child is over a year old
- Cough and cold medicines— I NEVER RECOMMEND THESE. They don’t really work well, if at all, and they’re particularly unsafe in children less than 4 years of age.
- Possible complications:
- Asthma attacks
- Sinus infection
- Ear infections
- Pneumonia
- If symptoms do not follow the typical course as described above, or your child has more severe or unusual symptoms (ear pain, difficulty breathing, prolonged symptoms more than 10 days, fever more than 5 days, higher fevers, vomiting, dehydration), take them to see a doctor.
- Prevention:
- Keep your child home and away from others while sick. The cold virus is shed from nose and throat secretions up to 7-10 days. Children are still contagious with cold symptoms even when they don’t have fever.
- HOWEVER, he can return to school contagious with cold symptoms if he’s fever-free. I know that makes no sense, but Texas Dept of State Health Services acknowledge we can’t keep kids home from school 10 days every time they have a cold. Hence, the frequent spread of colds at school.
- Wash hands frequently, disinfect frequently-touched items, and avoid close contact with others.
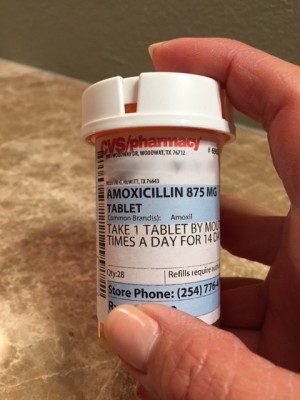
Common scenario: Kid has been sick with nasty green snot and a “deep wet cough” for 5 days. He’s cranky and tired, he’s bored from staying home from school for 3 days, and Mom is tired of wiping snot and staying up throughout the night. She wants to get it taken care of before it gets worse. She heads to the urgent care clinic, ER, or doctor’s office. They say her kid has a cold but give her “an antibiotic just in case.” Magically, the kid gets better in the next 2-3 days. Was it the antibiotic? NO. It’s just the natural course of the disease. He was at the peak of the illness and was going to get better within the next 2-5 days anyway. Don’t rush to get antibiotics. Don’t think “his colds always get better when he has amoxicillin.” Unless he had an accompanying ear infection or sinus infection or pneumonia, he didn’t need the antibiotic. It was just coincidental timing.
- STREP THROAT
- Cause: Group A strep bacteria
- Symptoms:
- Sore throat
- Fever, often over 101
- Headache
- Nausea or vomiting
- Enlarged lymph nodes
- Tonsils may be enlarged, red, or have white patches/pus
- Sandpapery red rash
- If a child comes in with just fever, headache, and nausea/vomiting (without sore throat), I will still test for strep and it’s often positive.
- Symptoms usually begin 2-5 days after being exposed to the bacteria through droplets/contact with secretions (coughing, sneezing, kissing, shaking hands, shared toys or items).
- Testing:
- Rapid strep test or throat culture
- Doctors can’t look at a throat and predict accurately if a strep test will be positive. Certain things greatly increase the likelihood (tiny red spots called petechiae on the roof of the mouth and red swollen tonsils with pus), but it’s still not a sure thing.
- Treatment:
- Penicillin shot or oral antibiotics
- Symptoms usually improve drastically after 24-48 hours of antibiotic
- No longer contagious after 24 hours of antibiotic
- Encourage lots of fluids, rest, Tylenol (acetaminophen) or Advil/Motrin (ibuprofen) for fever or pain.
- Possible complications:
- Most serious are acute rheumatic fever (inflammation of the heart) and acute glomerulonephritis (inflammation in the kidneys)
- Ear infections, pneumonia, sinus infection, throat or tonsil abscesses
- Prevention
- If your child has strep, keep him home until treated with antibiotics for 24 hours, then he may return to school.
- Wash hands frequently, disinfect frequently-touched items, and avoid close contact with others.
- INFLUENZA “THE FLU”
- Causes: Influenza A or B virus
- Symptoms: (first 3 often differentiate the flu from common cold)
- Sudden onset of illness
- High fever >101 and may get up to 104-105 (not all flu patients get fever), usually 3-5 days.
- Chills, muscle or body aches
- Headaches
- Runny nose, cough, sore throat, sneezing, stuffy nose
- Stomachaches
- Vomiting or diarrhea
- Fatigue and “not acting himself”
- Decreased appetite
- Symptoms usually begin 1-4 days after being exposed to the virus through droplets/contact with secretions (sneezing, coughing, kissing, shaking hands, shared toys or items). Symptoms get worse and peak around days 3-5, and usually last 7-14 days total.
- Testing:
- Rapid Flu test or Flu PCR, both with nasal swabs
- Treatment:
- Symptomatic treatment like colds: fluids, rest, Tylenol, Motrin, humidifier, saline/bulb suction, honey.
- Ibuprofen (Motrin/Advil) is particularly helpful with high fevers and muscle or body aches.
- Antiviral drugs, most common one is Oseltamivir (Tamiflu) for 5 days.
- Must be started within 2 days of getting sick
- Only shortens the illness by 1 day
- Decreases the severity of symptoms
- Helps prevent complications
- Very expensive (often $150-200 with insurance)
- Healthy children over 5 years old without underlying medical conditions and with mild symptoms do not need to take Tamiflu.
- Possible complications:
- Asthma attacks
- Sinus infection
- Ear infections
- Pneumonia
- Respiratory distress, hospitalization
- Prevention
- The flu is contagious beginning 1 day before symptoms develop and up to 7 days after symptoms start. So you guessed it! Your kid can and should go back to school when they’re fever-free and feeling mostly better, but they’re still likely contagious with their cough/sneezing.
- Get a flu vaccine! Flu shot for children 6 months and older.
- Wash hands frequently, disinfect frequently-touched items, and avoid close contact with others.
Hope this blog helps dispel some of the myths and half-truths associated with 3 of the most common winter illnesses seen in pediatric clinics. Use this as a guide, but always listen to your parental instincts. Take your child in to see a doctor if you have any concerns about their health.
Remember the common theme with prevention in all 3 illnesses: wash hands frequently and avoid close contact with others who are coughing/sneezing. Teach your kids to cough or sneeze into the bend of their arm to prevent spread of germs when they return to school.
Keep your kids healthy this holiday season and stay safe!
Soo Battle, M.D., F.A.A.P.
Disclaimer: The information contained on this website/blog is for informational purposes only and should not be used to replace the relationship that exists between you and your pediatrician or doctor. Please contact your doctor for medical advice and/or treatment recommendations specific to your child.